Chronic venous insufficiency
What is Chronic venous insufficiency (CVI)?
CVI is a condition when the venous wall and/or venous valves within the arteries of the legs are not working properly, making it difficult for the blood to return to the heart from the legs. This causes pooling of the blood in the leg veins and this pooling is called stasis.
How does the blood return to the heart from the legs?
The veins return blood low in oxygen because it has been used up by the tissues of the body. This blood has to return from the legs against gravity. When we walk the calf and foot muscles contract with each step squeezing the thin walled veins. To prevent the blood moving downwards due to the effect of gravity we have one-way valves in the leg veins.
Causes
-
In CVI these valves get damaged and allow the blood to leak backwards by gravity pull. The valves may get damaged due to aging or prolonged sitting or standing. When the valves in the veins are damaged it becomes difficult for the blood to move up the legs and it begins to stagnate increasing the pressure in the veins. This causes venous hypertension. This is CVI.
What causes CVI?
Symptoms
- Aging
- Prolonged sitting or standing
- DVT
- Pelvic tumours causing compression on the pelvic veins
- During late pregnancy when the uterus compresses the pelvic veins
- Vascular malformations
- Unknown cause.
Who are more prone to CVI?
-
Once the blood in the legs starts to stagnate it causes raised venous pressure called venous hypertension. This causes seepage of through the thin walled capillaries leading to leg swelling. The CVI that develops due to DVT is called post-thrombotic syndrome. 30% of the patients with DVT develop post-thrombotic syndrome within 10 years.
-
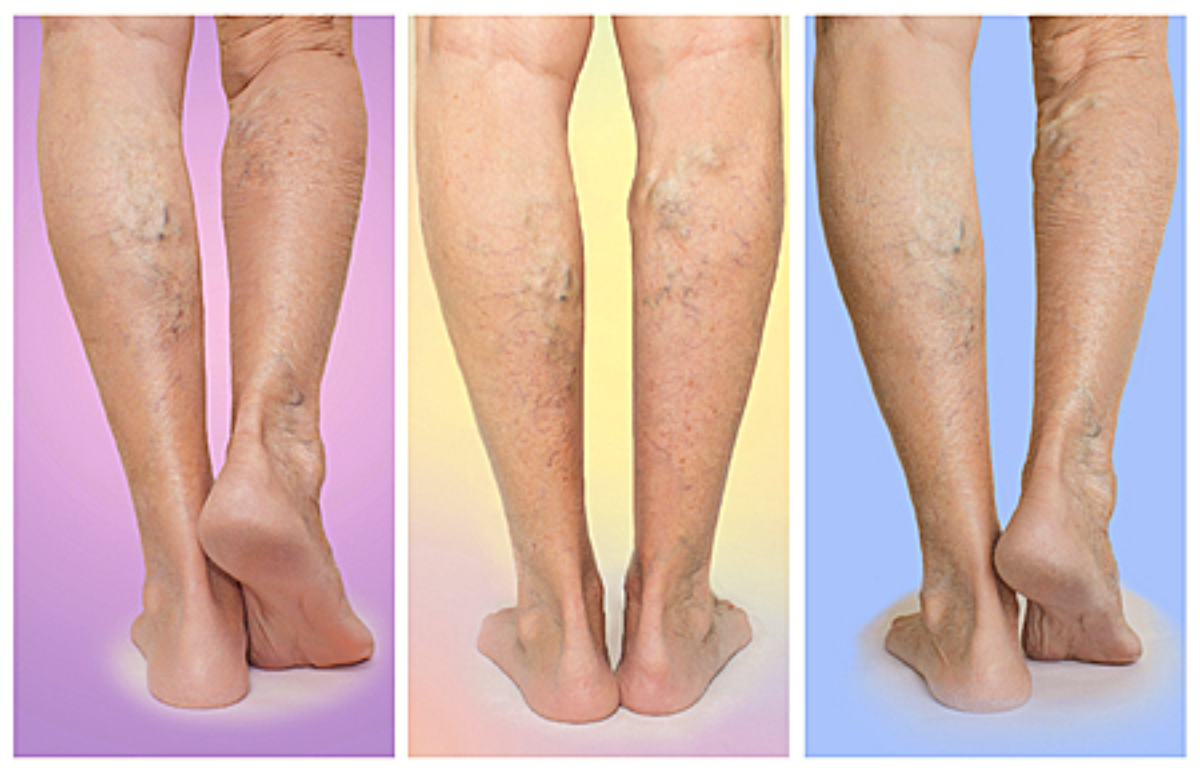
CVI worsens with the passage of time and the sooner it is treated, the better the chances of recovery. The problem will never go away by waiting. The symptoms include:
- Swelling in the ankles and lower legs worse after standing
- Ache or tiredness in the legs.
- New varicose veins
- Brown leathery skin of the lower legs
- Itching in the legs or feet
- Venous stasis ulcers.
-
In untreated cases the venous pressure rises to such high proportion that the fragile thinnest veins (capillaries) burst and the overlying skin becomes reddish brown in colour and is very sensitive to being broken if scratched or injured. The burst capillaries cause local tissue inflammation and internal tissue damage. This is the formation of ulcers which are difficult to heal and become infected. If still these are not treated they spread to the surrounding tissue and cause cellulitis. CVI leads to secondary varicose veins.
What happens in CVI?
How do the CVI patients present?
What happens in neglected cases?
Risk Factors
What are the risk factors for CVI?
These increase the chances of your developing CVI.
- Deep vein thrombosis
- Varicose veins
- Obesity
- Pregnancy
- Smoking
- Prolonged sitting or standing
- Females
- Advancing age over 50 years
Diagnosis
How is CVI diagnosed?
-
History and examination of the legs
-
Colour Doppler study of the venous system of the legs – this non-invasive test is patient friendly and has a very high success rate.
-
It is best treated early for good results and the goal of the treatment is to prevent pooling of the blood and leg ulcers. It is as follows:
-
Avoid prolonged sitting or standing
-
In long journeys keep flexing and extending your legs and ankles 10 times every 30 mins to keep the blood flowing through the leg veins
-
If you have a standing job take frequent breaks to sit down and elevate your legs.
-
Exercise regularly – walks
-
Lose weight if over weight
-
Wear compression stockings
-
Antibiotics if skin is infected
-
Practice good skin hygine
-
This is the main stay of the treatment of CVI along with leg elevation. The grade of compression varies from 8-10 mmHg and goes upto 40-50 mmHg. Your doctor will recommend what is suitable for you.
-
There is a role if cellulitis occurs or the patient develops infected ulcers.
-
may be given in post-thrombotic syndrome to prevent clot formation.
-
Multilayer compression dressings with topical wound care.
-
moisturizers are used to prevent cracking of the skin. If there are no cracks in the skin then anti-itch cream maybe used (hydrocortisone + zinc oxide) to protect skin. At times anti-fungal cream may be used to prevent fungal infection. Leaking skin is treated with wet compresses.
-
Sclerotherapy injection is needed in the small veins causing them to disappear after collapsing. It generally involves multiple sittings. It is inexpensive and a simple technique performed in the outpatients. By this the pain and discomfort of these veins is lost and complications like venous ulceration and hemorrhage are prevented.
-
In Radio-Frequency Ablation (RFA) there is intense local heat within the vein ablating it. The targeted veins are closed shut but left in place to prevent excessive bruising. The patients return to normal activity the next day.
-
Healthy veins are removed from elsewhere in the body to re-route the blood around the veins affected by CVI. This only done as a last resort when all other options have been exhausted.
-
Eat a healthy balanced diet
-
Quit smoking
-
Exercise regularly
-
Avoid wearing restrictive clothing like tight girdles and belts.
-
Lose weight if over weight
-
Avoid prolonged sitting or standing.
-
Content Reviewed by - Dr. Jaisom Chopra
Treatment
How is CVI treated?
Do compression stockings help?
Do drugs help?
Antibiotics –
Anticoagulation –
Skin care –
Is sclerotherapy and RFA indicated in CVI?
Is bypass surgery an option?
Can CVI be prevented?
The only way is to reduce the risk factors by following the following guidelines.